| ||||
|
|
|
|
| ||||
|
|
|
|
|
| ||||||||||||||||||
INTRODUCTION AND OVERVIEW |
||||||||||||||||||
|
There are many different quantities and units used to quantify radiation, because there are a number of different aspects of an x-ray beam or gamma radiation that can be used to express the amount of radiation. The selection of the most appropriate quantity depends on the specific application. The primary objective of this chapter is to help the reader develop a conceptual understanding of the various radiation quantities and units and gain sufficient factual knowledge to support their usage.
|
||||||||||||||||||
UNIT SYSTEMS |
||||||||||||||||||
|
A complicating factor is that American society is undergoing a slow change in the units used to express a variety of physical quantities. In everyday life we see this as a change from the conventional British unit system (feet, pounds, miles) to the metric system (meters, kilograms, kilometers). In radiology we are experiencing a change not only to the general metric units but also to the proposed adoption of a set of fundamental metric units known as the International System of Units (SI units). The adoption of SI radiation units is progressing rather slowly because there is nothing wrong with our conventional units, and SI units are somewhat awkward for a number of common applications. Throughout this text we use the units believed the most useful to the reader. In this chapter both unit systems are discussed and compared. The table below is a listing of most of the physical quantities and units encountered in radiology. It is a useful reference especially for the conversion of one system of units to another.
| ||||||||||||||||||
| Exposure | Conventional Unit | SI Unit | Conversions |
| Exposure | roentgen (R) | coulomb/kg of air (C/kg) | 1 C/kg = 3876 R |
| 1 R = 258 uC/kg | |||
| Dose | rad (R) | gray (Gy) | 1 Gy = 100 rad |
| Dose equivalent | rem | sievert (Sv) | 1 Sv = 100 rem |
| Activity | curie (Ci) | becquerel (Bq) | 1 mCi = 37 mBq |
QUANTITIES |
||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
 | ||||||||||||||||||
|
Radiation Quantities and Units | ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
 | ||||||||||||||||||
|
Inverse-Square Effect | ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
|
||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
PHOTONS |
||||||||||||||||||
|
Since an x-ray beam and gamma radiation are showers of individual photons, the number of photons could, in principle, be used to express the amount of radiation. In practice, the number of photons is not commonly used, but it is a useful concept in understanding the nature of radiation and distinguishing between concentration and total radiation. Let us go back to the situation shown above and examine the different ways the concentration of radiation delivered to a small area on a patient's body could be expressed. |
||||||||||||||||||
|
| ||||||||||||||||||
Photon Concentration (Fluence) |
||||||||||||||||||
|
If we draw a 1- cm2 area on the surface of the patient and then count the number of photons passing through the area during a radiographic procedure, we will have an indication of the concentration of radiation delivered to the patient. During a single abdominal radiographic exposure we would find that close to 1010 photons would have passed through our square centimeter. The more formal term for photon concentration is photon fluence.
| ||||||||||||||||||
Total Photons |
||||||||||||||||||
|
If we count the number of photons entering the total exposed area, we will have an indication of the total amount of radiation energy delivered to the patient. This quantity depends on the size of the exposed area and the radiation concentration. If the radiation is uniformly distributed over the exposed area, the total number of photons entering the patient can be found by multiplying the concentration (fluence) by the exposed area. Changing the size of the exposed area does not affect the concentration entering at the center of the beam. However, reducing the exposed area does reduce the total number of photons and radiation entering the patient. | ||||||||||||||||||
|
| ||||||||||||||||||
EXPOSURE |
||||||||||||||||||
|
| ||||||||||||||||||
Concept | ||||||||||||||||||
|
Exposure is the quantity most commonly used to express the amount of radiation delivered to a point. The conventional unit for exposure is the roentgen (R), and the Sl unit is the coulomb per kilogram of air (C/kg): | ||||||||||||||||||
|
| ||||||||||||||||||
|
1 R = 2.58 x 10-4 C/kg | ||||||||||||||||||
|
1 C/kg = 3876 R | ||||||||||||||||||
|
The reason exposure is such a widely used radiation quantity is that it can be readily measured. All forms of radiation measurement are based on an effect produced when the radiation interacts with a material. The specific effect used to measure exposure is the ionization in air produced by the radiation. | ||||||||||||||||||
|
| ||||||||||||||||||
|
 | ||||||||||||||||||
|
Exposure | ||||||||||||||||||
|
| ||||||||||||||||||
|
Exposure is generally measured by placing a small volume of air at the point of measurement and then measuring the amount of ionization produced within the air. The enclosure for the air volume is known as an ionization chamber. The use of ionization chambers and other radiation measuring devices is discussed in Chapter 42. The concept of exposure and its units can be developed from the figure above. When a small volume of air is exposed to ionizing radiation (x-ray, gamma, etc.), some of the photons will interact with the atomic shell electrons. The interaction separates the electrons from the atom, producing an ion pair. When the negatively charged electron is removed, the atom becomes a positive ion. Within a specific mass of air the quantity of ionizations produced is determined by two factors: the concentration of radiation photons and the energy of the individual photons. | ||||||||||||||||||
|
| ||||||||||||||||||
|
An exposure of 1 roentgen produces 2.08 x 109 ion pairs per cm3 of air at standard temperature and pressure (STP); 1 cm3 of air at STP has a mass of 0.001293 g. The official definition of the roentgen is the amount of exposure that will produce 2.58 x 10-4 C (of ionization) per kg of air. A coulomb is a unit of electrical charge. Since ionization produces charged particles (ions), the amount of ionization produced can be expressed in coulombs. One coulomb of charge is produced by 6.24 x 1018 ionizations. | ||||||||||||||||||
|
| ||||||||||||||||||
|
Exposure is a quantity of radiation concentration. For a specific photon energy, exposure is proportional to photon concentration or fluence. The relationship between exposure and photon concentration is shown below; the relationship changes with photon energy because both the number of photons that will interact and the number of ionizations produced by each interacting photon is dependent on photon energy. If we assume a photon energy of 60 keV, a 1-R exposure is equivalent to a concentration of approximately 3 x 1010 photons per cm2. | ||||||||||||||||||
|
| ||||||||||||||||||
|
 | ||||||||||||||||||
|
Relationship between Exposure and Photon Concentration
| ||||||||||||||||||
AIR KERMA |
||||||||||||||||||
|
Air kerma is another radiation quantity
that is sometimes used to express the radiation concentration delivered to
a point, such as the entrance surface of a patient's body. It
is a quantity that fits into the SI scheme. | ||||||||||||||||||
|
| ||||||||||||||||||
| The quantity, kerma, originated from
the acronym, KERMA, for Kinetic Energy Released per unit MAss (of
air). It is a measure of the amount of radiation energy, in the unit
of joules (J), actually deposited in or absorbed in a unit mass (kg) of
air. Therefore, the quantity, kerma, is expressed in the units of
J/kg which is also the radiation unit, the gray (G) . A little later
we are going to discover that the concentration of radiation energy
absorbed in a material is actually the radiation quantity, Absorbed
Dose , but more on that later. At this time we just need to recognize
that air kerma is just the Absorbed Dose in air.
The quantity, air kerma, has two things going
for it and is beginning to replace the quantity, exposure, for expressing
the concentration of radiation delivered to a point, like the entrance
surface to a human body (patient or staff). | ||||||||||||||||||
|
| ||||||||||||||||||
| 1. It is easy to measure with an ionization
chamber. Since the ionization produced in air by radiation is
proportional to the energy released in the air by the radiation,
ionization chambers actually measure air kerma as well as exposure.
An ionization chamber can be calibrated to read air kerma, or a conversion
factor can be used to convert between air kerma and exposure
values. | ||||||||||||||||||
|
| ||||||||||||||||||
| 2. It is expressed in a practical metric SI
unit. Air kerma (energy released in a unit
mass of air) is expressed in the units of joule per kilogram, J/kg.
This is also the unit gray, Gy, used for absorbed dose. Here is the
easy part. If we know air kerma measured (or calculated) at a point
where soft tissue is located, the absorbed dose in the tissue will be just
about equal to the air kerma.
| ||||||||||||||||||
Surface Integral Exposure |
||||||||||||||||||
|
Since exposure expressed in roentgens or coulombs per kilogram is a concentration, it does not express the total amount of radiation delivered to a body. The total radiation delivered, or surface integral exposure (SIE), is determined by the exposure and the dimensions of the exposed area. It is also referred to as the exposure-area product. | ||||||||||||||||||
|
| ||||||||||||||||||
|
The surface integral exposure is expressed in the conventional units of roentgens-square centimeters (R-cm2). If the radiation exposure is uniform over the entire area, the SIE is the product of the exposure in roentgens and the exposure area in square centimeters. If the exposure is not the same at all points in the exposed area, the SIE can be found by adding the exposure values for each square centimeter of exposed surface. Mathematically, this is the process of integrating the exposure over the surface area. The SIE can be measured during x-ray examinations by placing a special type of ionization chamber in the x-ray beam. The significance of SIE is that it describes total radiation imparted to a patient, whereas exposure indicates only the concentration of radiation at a specified point. | ||||||||||||||||||
|
| ||||||||||||||||||
|
The typical fluoroscopy examination provides an excellent opportunity to compare exposure (concentration) and SIE (total radiation). In the figure below two cases are compared. In both instances the beam area was 10 cm x 10 cm (100 cm2); the total exposure time was 5 minutes at an exposure rate of 3 R/min. In both instances the SIE is 1,500 R- cm2. However, the exposure depends on how the x-ray beam was moved during the examination. In the first example the beam was not moved and the resulting exposure was 15 R. In the second example, the beam was moved to different locations so that the exposure was distributed over more surface area and the concentration became less. | ||||||||||||||||||
|
| ||||||||||||||||||
|
 | ||||||||||||||||||
|
Comparison of SIE and Exposure during a Fluoroscopic
Examination | ||||||||||||||||||
|
| ||||||||||||||||||
|
Another important example is illustrated below. Here the same exposure (100 mR) is delivered to both patients. However, there is a difference in the exposed area: the patient on the right received 10 times as much radiation as the patient on the left. | ||||||||||||||||||
|
| ||||||||||||||||||
|
 | ||||||||||||||||||
|
Comparison of SIE Values for a Radiographic Examination
| ||||||||||||||||||
Dose Area Product (DAP) |
||||||||||||||||||
| Dose Area Product (DAP) is similar in concept to surface integral exposure and exposure area product in that they all express total radiation delivered to a patient. The principle difference is in the units used. DAP is in dose units, such as Gy-cm2. For a uniformly exposed area, the DAP is just the product of the air kerma, in Gy or mGy, and the exposed area in cm2. DAP provides a good estimation of the total radiation energy delivered to a patient during a procedure. Both radiographic and fluoroscopic machines can be equipped with devices (DAP meters) or computer programs that measure or calculate the DAP for each procedure. It is the most practical quantity for monitoring the radiation delivered to patients. | ||||||||||||||||||
|
The important point to remember is that exposure (roentgens) alone does not express the total radiation delivered to a body. The total exposed area must also be considered. | ||||||||||||||||||
|
| ||||||||||||||||||
ENERGY |
||||||||||||||||||
|
An x-ray beam and other forms of radiation deliver energy to the body. In principle, the amount of radiation delivered could be expressed in units of energy (joules, ergs, kiloelectron volts, etc.). The energy content of an x-ray beam is rather difficult to measure and for that reason is not widely used in the clinical setting. However, considering the energy delivered by an x-ray beam is helpful in understanding other radiation quantities. | ||||||||||||||||||
|
| ||||||||||||||||||
Energy Fluence |
||||||||||||||||||
|
| ||||||||||||||||||
|
Energy fluence (concentration) is the amount of radiation energy delivered to a unit area. The units for expressing radiation energy concentration are either the millijoule (mJ) per square centimeter or erg per square centimeter. For a specific photon energy, fluence is proportional to exposure. The relationship between energy fluence and exposure is shown above, under "EXPOSURE". The relationship changes with photon energy because of the change in photon interaction rates. However, if we assume a photon energy of 60 keV, the energy fluence for a 1-R exposure is approximately 0.3 mJ/ cm2. | ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
The energy delivered by an x-ray beam can be put into perspective by comparing it to the energy delivered by sunlight, as shown below. For the x-ray exposure we will use the fluoroscopic factors of 5 minutes at the rate of 3 R/min. This 15-R exposure delivers x-ray energy to the patient with a concentration (fluence) of 4.5 mJ/cm2 if we assume an effective photon energy of 60 keV. | ||||||||||||||||||
|
| ||||||||||||||||||
|
 | ||||||||||||||||||
|
Comparison of Energy Delivered by an X-Ray Beam and
Sunlight | ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
The energy delivered by the sun depends on many factors including geographic location, season, time of day, and atmospheric conditions; a typical midday summer exposure on a clear day in Atlanta produces approximately 100 mJ/sec/cm2. In 5 minutes a person would be exposed to an energy fluence of 30,000 MJ/cm2. We see from this example that the energy content of an x-ray beam is relatively small in comparison to sunlight. However, x-ray and gamma radiation will generally produce a greater biological effect per unit of energy than sunlight because of two significant differences: x- and gamma radiation penetrate and deposit energy within the internal tissue, and the high energy content of the individual photons produces a greater concentration of energy at the points where they are absorbed within individual atoms. | ||||||||||||||||||
|
| ||||||||||||||||||
Total Energy | ||||||||||||||||||
|
| ||||||||||||||||||
|
The total energy imparted to a body by an x-ray beam is determined by the energy fluence (concentration) and the size of the exposed area. If the radiation is uniformly distributed over the area, the total energy delivered is the product of the fluence and the surface area. | ||||||||||||||||||
|
| ||||||||||||||||||
ABSORBED DOSE |
||||||||||||||||||
|
| ||||||||||||||||||
Concept | ||||||||||||||||||
|
| ||||||||||||||||||
|
A human body absorbs most of the radiation energy delivered to it. The portion of an x-ray beam that is absorbed depends on the penetrating ability of the radiation and the size and density of the body section exposed. In most clinical situations more than 90% is absorbed. In nuclear imaging procedures, a large percentage of the energy emitted by radionuclides is absorbed in the body. Two aspects of the absorbed radiation energy must be considered: the amount (concentration) absorbed at various locations throughout the body and the total amount absorbed. | ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
Absorbed dose is the quantity that expresses the concentration of radiation energy absorbed at a specific point within the body tissue. Since an x-ray beam is attenuated by absorption as it passes through the body, all tissues within the beam will not absorb the same dose. The absorbed dose will be much greater for the tissues near the entrance surface than for those deeper within the body. Absorbed dose is defined as the quantity of radiation energy absorbed per unit mass of tissue. | ||||||||||||||||||
|
| ||||||||||||||||||
Units | ||||||||||||||||||
|
The conventional unit for absorbed dose is the rad, which is equivalent to 100 ergs of absorbed energy per g of tissue. The SI unit is the gray (Gy), which is equivalent to the absorption of 1 J of radiation energy per kg of tissue. The relationship between the two units is | ||||||||||||||||||
|
| ||||||||||||||||||
|
1 rad = 100 erg/g = 0.01 J/kg = 0.01 Gy | ||||||||||||||||||
|
1 Gy = 100 rad | ||||||||||||||||||
|
For a specific type of tissue and photon energy spectrum, the absorbed dose is proportional to the exposure delivered to the tissue. The ratio, f, between dose (rads) and exposure (roentgens) is shown below for soft tissue and bone over the photon energy range normally encountered in diagnostic procedures. The absorbed dose in soft tissue is slightly less than 1 rad/R of exposure throughout the photon energy range. The relationship for bone undergoes a considerable variation with photon energy. For a typical diagnostic x-ray spectrum, a bone exposure of 1 R will produce an absorbed dose of approximately 3 rad. | ||||||||||||||||||
|
| ||||||||||||||||||
|
 | ||||||||||||||||||
|
Relationship of Absorbed Dose to
Exposure | ||||||||||||||||||
Computed Tomography Dose Index (CTDI) |
||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
The Concept of Computed Tomography Dose
Index (CTDI) | ||||||||||||||||||
|
The Computed Tomography Dose
Index, CTDI, is the special dose quantity that is used extensively to
express absorbed dose in CT. | ||||||||||||||||||
|
| ||||||||||||||||||
| Let's recall that in CT the
x-ray beam is rotated around the patient and passes through from all
sides. This gives a relatively uniform distribution of absorbed dose
within each slice. A dose value determined at the center of the
slice is usually considered a good indicator of tissue dose and can be
used to compare imaging techniques and for dose management purposes.
One of the complicating factors in determining CT dose is that the tissue
in a slice is exposed to two sources of x-radiation. One is the
direct beam and the other is the scattered radiation from adjacent slices
in the typical multiple slice imaging procedure. It is the contribution
from the scattered radiation that is very difficult to measure.
Values for the CTDI are determined by a measuring protocol that makes a
reasonable estimate of the dose contribution from scatter. The
typical procedure is illustrated above. A pencil shaped dosimeter
(ionization chamber) is placed in a phantom. It is then scanned for
only one complete slice and the dose value is read. The dosimeter
will read the radiation from the direct x-ray beam within the
slice plus the scattered radiation coming out of the sides of the
slice and reaching the dosimeter. Here is a somewhat subtle but
crucial point: the concept of the CTDI is based on the assumption that the
scatter measured from a single slice, as just described, is a good
estimate of the scatter into a slice from adjacent slices in a
multiple-slice scan. This procedure does provide a good
approximation of the actual dose, but since it is not completely precise,
it is called a dose index. | ||||||||||||||||||
|
| ||||||||||||||||||
| The CTDI can be measured at points
other than the center of a slice, if that information is
needed.
| ||||||||||||||||||
Mean Glandular Dose (MGD) |
||||||||||||||||||
|
| ||||||||||||||||||
|
Mean Glandular Dose (MGD) in the
Breast | ||||||||||||||||||
|
The Mean Glandular Dose (MGD)
is the special dose quantity used in mammography. It is defined as
the mean, or average, dose to the glandular tissue within the
breast. The assumption is that the glandular tissue, and not the
fat, is the tissue at risk from radiation exposure. Obviously, it is
just about impossible to determine the actual dose to the glandular tissue
during a specific mammographic procedure because of variations in breast
size and distribution of glandular tissue within the breast. The MGD
is based on some standard breast parameters. | ||||||||||||||||||
|
| ||||||||||||||||||
|
MGD values are determined by
following a standard two-step protocol: | ||||||||||||||||||
|
| ||||||||||||||||||
|
1. The first step is to
determine the entrance surface exposure, or air kerma, to the
breast. This can be measured directly with small dosimeters placed
on the breast or calculated from the known calibration factors for the
mammography equipment. | ||||||||||||||||||
|
| ||||||||||||||||||
|
2. Then, the MGD is determined by multiplying the surface exposure value by published dose factors. The dose factor values are tabulated according to breast size and composition and the penetrating characteristics of the x-ray beam as determined by the anode material, filtration, and KV. For comparison of imaging techniques, evaluation of equipment performance, general dose management, and regulatory and accreditation purposes, the MGD to a "standard" breast is used. The standard is a 4.2cm thick compressed breast consisting of 50% glandular tissue and 50% fat. This corresponds to the standard phantom that is used for image quality evaluation and comparative dose determinations.
| ||||||||||||||||||
|
| ||||||||||||||||||
Integral Dose |
||||||||||||||||||
|
Integral dose is the total amount of energy absorbed in the body. It is determined not only by the absorbed dose values but also by the total mass of tissue exposed. | ||||||||||||||||||
|
| ||||||||||||||||||
|
The conventional unit for integral dose is the gram-rad, which is equivalent to 100 ergs of absorbed energy. The concept behind the use of this unit is that if we add the absorbed doses (rads) for each gram of tissue in the body, we will have an indication of total absorbed energy. Since integral dose is a quantity of energy, the SI unit used is the joule. The relationship between the two units is | ||||||||||||||||||
|
| ||||||||||||||||||
|
1 J = 1,000 gram-rad | ||||||||||||||||||
|
Integral dose (total absorbed radiation energy) is probably the radiation quantity that most closely correlates with potential radiation damage during a diagnostic procedure. This is because it reflects not only the concentration of the radiation absorbed in the tissue but also the amount of tissue affected by the radiation. | ||||||||||||||||||
|
| ||||||||||||||||||
|
There is no practical method for measuring integral dose in the human body. However, since most of the radiation energy delivered to a body is absorbed, the integral dose can be estimated to within a few percent from the total energy delivered to the body. | ||||||||||||||||||
|
| ||||||||||||||||||
|
Computed tomography can be used to demonstrate integral dose, as illustrated below. We begin with a one-slice examination and assume that the average dose to the tissue in the slice is 5 rad. If there are 400 g of tissue in the slice, the integral dose will be 2,000 gram-rad. If we now perform an examination of 10 slices, but all other factors remain the same, the dose (energy concentration) in each slice will remain the same. However, the integral dose (total energy) increases in proportion to the number of slices and is now 20,000 gram-rad. In this example we made the simplifying assumption that no radiation is scattered from one slice to another. In reality, some radiation is exchanged between contiguous slices but that does not affect the concept presented. | ||||||||||||||||||
|
| ||||||||||||||||||
|
 | ||||||||||||||||||
|
| ||||||||||||||||||
|
Integral Dose in Computed Tomography
| ||||||||||||||||||
Dose Length Product (DLP) |
||||||||||||||||||
|
| ||||||||||||||||||
|
The Concept of Dose Length Product | ||||||||||||||||||
|
We recall that the CTDI is the practical quantity for specifying dose in CT procedures. The associated quantity for specifying the "total radiation" to a patient is the dose length product (DLP) as illustrated here. The DLP is just the product of the CTDI value and the length of the body area scanned. It has the units of either rad-cm or Gy-cm. It is a useful and practical quantity for comparing the total radiation to patients for various CT procedures. It is, however, not a precise measure of the total radiation or integral dose; that is more difficult to determine. | ||||||||||||||||||
BIOLOGICAL IMPACT |
||||||||||||||||||
|
It is sometimes desirable to express the actual or relative biological impact of radiation. It is necessary to develop a distinction between the biological impact and the physical quantity of radiation because all types of radiation do not have the same potential for producing biological change. For example, one rad of one type of radiation might produce significantly more radiation damage than one rad of another type. In other words, the biological impact is determined by both the quantity of radiation and its ability to produce biological effects. Two radiation quantities are associated with biological impact. | ||||||||||||||||||
|
| ||||||||||||||||||
Dose Equivalent |
||||||||||||||||||
|
Dose equivalent (H) is the quantity commonly used to express the biological impact of radiation on persons receiving occupational or environmental exposures. Personnel exposure in a clinical facility is often determined and recorded as a dose equivalent. | ||||||||||||||||||
|
| ||||||||||||||||||
|
Dose equivalent is proportional to the absorbed dose (D), the quality factor (Q), and other modifying factors (N) of the specific type of radiation. Most radiations encountered in diagnostic procedures (x-ray, gamma, and beta) have quality and modifying factor values of 1. Therefore, the dose equivalent is numerically equal to the absorbed dose. Some radiation types consisting of large (relative to electrons) particles have quality factor values greater than 1. For example, alpha particles have a quality factor value of approximately 20. | ||||||||||||||||||
|
| ||||||||||||||||||
|
The conventional unit for dose equivalent is the rem, and the Sl unit is the sievert (Sv). When the quality factor is 1, the different relationships between dose equivalent (H) and absorbed dose (D) are | ||||||||||||||||||
|
H(rem) = D(rad) | ||||||||||||||||||
|
H(Sv) = D(Gy). | ||||||||||||||||||
|
| ||||||||||||||||||
|
Dose equivalent values can be converted from one system of units to the other by: | ||||||||||||||||||
|
| ||||||||||||||||||
|
1 Sv = 100 rem. | ||||||||||||||||||
|
The figure below is a summary of the general relationship among the three quantities: exposure, absorbed dose, and dose equivalent. Although each expresses a different aspect of radiation, they all express radiation concentration. For the types of radiation used in diagnostic procedures, the factors that relate the three quantities have values of approximately 1 in soft tissue. Therefore, an exposure of 1 R produces an absorbed dose of approximately 1 rad, which, in turn, produces a dose equivalent of 1 rem. | ||||||||||||||||||
|
| ||||||||||||||||||
|
 | ||||||||||||||||||
|
Relationship of Exposure, Absorbed Dose, and Dose
Equivalent | ||||||||||||||||||
|
| ||||||||||||||||||
Relative Biological Effectiveness |
||||||||||||||||||
|
When specific radiation effects rather than general risk are being considered, the relative biological effectiveness (RBE) of the radiation must be taken into account. The value of the RBE depends on characteristics of the radiation and the specific biological effects being considered. This radiation characteristic is generally not used in association with diagnostic procedures. Additional discussions of the concept can be found in radiation biology texts.
| ||||||||||||||||||
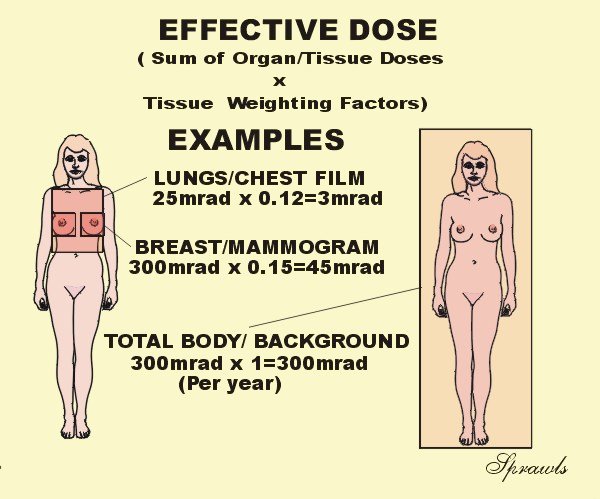
Effective Dose |
||||||||||||||||||
|
| ||||||||||||||||||
|
 | ||||||||||||||||||
|
The Concept of Effective Dose | ||||||||||||||||||
|
Effective dose is becoming a very useful radiation quantity for expressing relative risk to humans, both patients and other personnel. It is actually a simple and very logical concept. It takes into account the specific organs and areas of the body that are exposed. The point is that all parts of the body and organs are not equally sensitive to the possible adverse effects of radiation, such as cancer induction and mutations. For the purpose of determining effective dose, the different areas and organs have been assigned tissue weighting factor (wT) values. For a specific organ or body area the effective dose is: | ||||||||||||||||||
|
Effective Dose (Gy) = Absorbed Dose (Gy) x | ||||||||||||||||||
|
If more than one area has
been exposed, then the total body effective dose is just the sum of the
effective doses for each exposed area. It is a simple as that.
Now let's see why effective dose is such a useful quantity. There is
often a need to compare the amount of radiation received by patients for
different types of x-ray procedures, for example, a chest radiograph and a
CT scan. The effective dose is the most appropriate quantity for
doing this. Also, by using effective dose it is possible to put the
radiation received from diagnostic procedures into perspective with other
exposures, especially natural background radiation. It is generally assumed that
the exposure to natural background radiation is somewhat uniformly
distributed over the body. Since the tissue weighting factor for the
total body has the value of one (1), the effective dose is equal to the
absorbed dose. This is assumed to be 300 mrad in the
illustration. Let's look at an
illustration. If the the dose to the breast, MGD, is 300 mrad for
two views, the effective dose is 45 mrad because the tissue weighting
factor for the breast is 0.15. *For the remaining organs a value of 0.06 is
used for each of the five organs receiving the highest dose. | ||||||||||||||||||
LIGHT |
||||||||||||||||||
|
The basic light quantities and units encountered in radiology can be conveniently divided into two categories: those that express the amount of light emitted by a source and those that describe the amount of light falling on a surface, such as a piece of film. The relationships of several light quantities and units are shown below. | ||||||||||||||||||
|
 | ||||||||||||||||||
|
Light Quantities and Units Encountered in Radiology
| ||||||||||||||||||
|
| ||||||||||||||||||
Luminance |
||||||||||||||||||
|
Luminance is the light quantity generally referred to as brightness. It describes the amount of light being emitted from the surface of the light source. The basic unit of luminance (brightness) is the nit, which is equivalent to 1 candela per m2 of source area. | ||||||||||||||||||
|
| ||||||||||||||||||
|
The concept of luminance is somewhat easier to understand if it is related to the number of light photons involved. The quantity for specifying an amount of light is the lumen. One lumen of light with wavelengths encountered in x-ray imaging systems (540 nm) is equivalent to 3.8 x 1015 photons per second. Another factor that determines luminance is the concentration of light in a given direction. This can be described in terms of a cone or solid angle that is measured in units of steradians (sr). | ||||||||||||||||||
|
| ||||||||||||||||||
|
If a light source produces an intensity of 1 cd/m2 of surface area, it has a luminance of 1 nit. Perhaps it is more realistic to consider the quantity of light that would be emitted from a 1-mm2 area of a source, such as the output screen of an image intensifier. One millimeter square is 10-6 m2. If the intensifier has a luminance (brightness) of 1 nit, the intensity from an area of 1 mm2 would be 10-6 lumen in a 1-unit solid angle. This would be equivalent to 3.8 x 109 photons per second, leaving the 1-mm2 area through a cone (solid angle) of 1 sr of source area. | ||||||||||||||||||
|
| ||||||||||||||||||
|
Viewbox and other image display device brightness is measured in the units of nits. It is generally in the range of 1,500 nits to 2,000 nits for most image viewing except mammography, where it should be at least 3,500 nits. | ||||||||||||||||||
|
| ||||||||||||||||||
|
Another unit used for specifying luminance is the foot-lambert, which is equivalent to 3.426 nits. | ||||||||||||||||||
|
| ||||||||||||||||||
Illuminance |
||||||||||||||||||
|
Illuminance is a specification of the quantity of light falling on or illuminating a surface. The basic unit is the lux. A surface has an illuminance of 1 lux when it receives 1 lumen/m2 of surface area. Consider a small area on a piece of film that is 1 mm2. For light with a wavelength of 540 nm, there are 3.8 x 1015 photons per second per lumen. An illuminance to the film of 1 lux would be equivalent to 3.8 x 102 photons per sec to a 1-mm2 area. The total light exposure to a film is found by multiplying the illuminance, in lux, by the exposure time, in seconds, and is expressed in units of lux-seconds. | ||||||||||||||||||
|
| ||||||||||||||||||
|
Another unit used in some literature for specifying illuminance is the footcandle, which is equivalent to 10.764 lux. | ||||||||||||||||||
|
| ||||||||||||||||||
RADIO FREQUENCY RADIATION |
||||||||||||||||||
|
Radio frequency (RF) radiation is used in magnetic resonance imaging (MRI). During an imaging procedure, pulses of RF energy are applied to the patient's body where most of it is absorbed. Conventional energy units are used to express the amount of RF energy imparted to the body. | ||||||||||||||||||
|
| ||||||||||||||||||
|
Power is the rate at which energy is transferred. The unit for power is the watt, which is equivalent to an energy transfer at the rate of 1 joule/second. During the acquisition phase of MRI, the system transfers energy to the patient's body at some specific power level. The actual power (watts) used depends on many factors associated with the examination. | ||||||||||||||||||
|
| ||||||||||||||||||
Specific Absorption Rate (SAR) |
||||||||||||||||||
|
From the standpoint of effect on the patient's body a more significant quantity is the concentration of power in the tissue. This is expressed in the units of watts per kilogram of tissue and is designated the specific absorption rate (SAR). Since RF energy is not uniformly distributed within the body, two quantities must be considered: the SAR in a specific location and the average SAR within the total body. The RF energy absorbed by the tissue is converted into heat. Therefore, the power concentration is an indication of the rate at which heat is produced within specific tissue. | ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||
|
| ||||||||||||||||||