
Chapter 1
Magnetic Resonance Image Characteristics
 |
Chapter 1 |
| Link to Book Table of Contents | Chapter Contents Shown Below |
Magnetic resonance imaging (MRI) is a medical imaging
process that uses a magnetic field and radio frequency (RF) signals to produce
images of anatomical structures, of the presence of disease, and of various
biological functions within the human body. MRI produces images that are
distinctly different from the images produced by other imaging modalities. A
primary difference is that the MRI process can selectively image several
different tissue characteristics. A potential advantage of this is that if a
pathologic process does not alter one tissue characteristic and produce
contrast, it might be visible in an image because of its effect on other
characteristics. This causes the MRI process to be somewhat more complex than
most imaging methods. In order to optimize an MRI procedure for a specific
clinical examination, the user must have a good knowledge of the characteristics
of the magnetic resonance (MR) image and how those characteristics can be
controlled.
In this chapter we will develop a basic
knowledge and overview of the MR image, how the image relates to specific tissue
characteristics, and how image quality characteristics can be controlled.
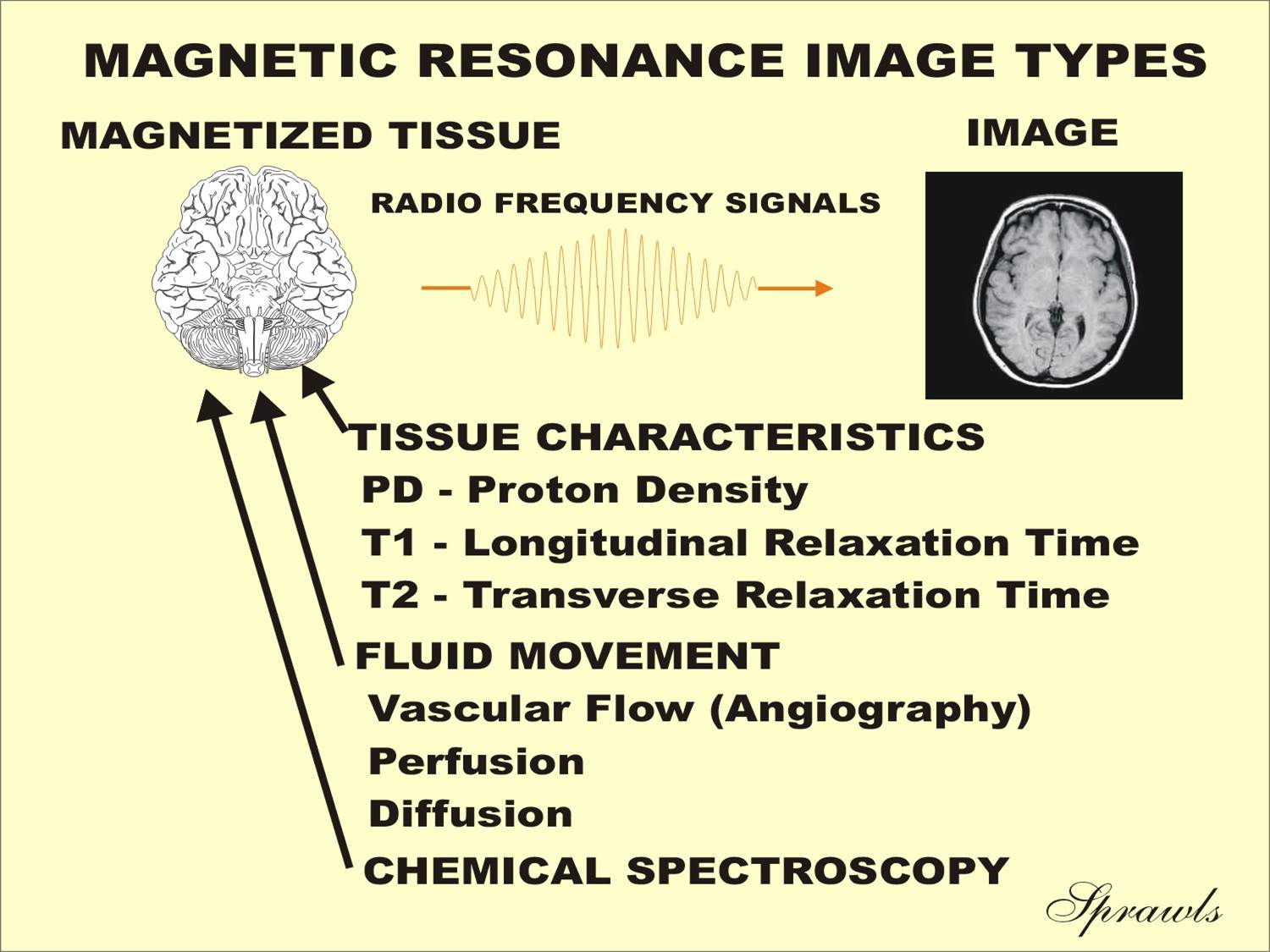
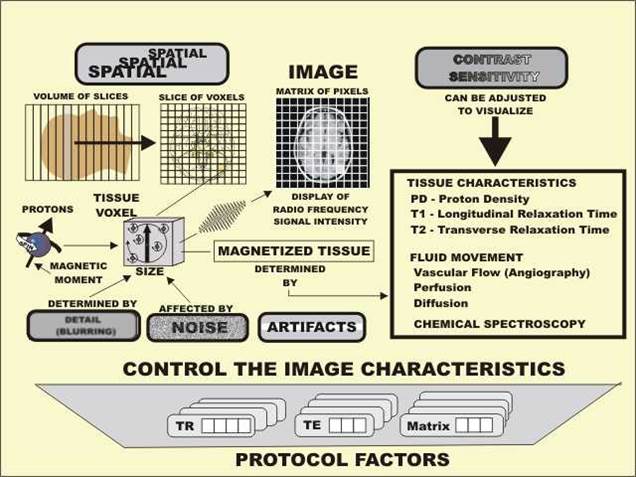
The MR image displays certain physical characteristics of
tissue. Let us now use Figure 1-1 to identify these characteristics and to see
how they are related.
|
Figure 1-1. Physical characteristics of tissue and fluid movement that
can be displayed in the magnetic resonance image. |
 |
The MR image is a display of RF signals that are
emitted by the tissue during the image acquisition process. The source of the
signals is a condition of magnetization that is produced in the tissue when the
patient is placed in the strong magnetic field. The tissue magnetization depends
on the presence of magnetic nuclei. The specific physical characteristic of
tissue or fluid that is visible in the image depends on how the magnetic field
is being changed during the acquisition process. An image acquisition consists
of an acquisition cycle, like a heartbeat, that is repeated many times. During
each cycle the tissue magnetization is forced through a series of changes. As we
will soon learn in much more detail, all tissues and fluids do not progress
through these changes at the same rate. It is the level of magnetization that is
present at a special “picture snapping time” at the end of each cycle that
determines the intensity of the RF signal produced and the resulting tissue
brightness in the image.
MR images are generally identified with
specific tissue characteristics or blood conditions that are the predominant
source of contrast. These characteristics determine the level of tissue
magnetization and contrast present at the time the “picture is snapped.” The
equipment operator, who sets the imaging protocol, determines the type of image
that is to be produced by adjusting various imaging factors.
The characteristics that can be used as a
source of image contrast fall into three rather distinct categories. The first,
and most widely used, category is the magnetic characteristics of tissues. The
second category is characteristics of fluid (usually blood) movement. The third
category is the spectroscopic effects related to molecular structure.
At this time we will briefly introduce each of
these characteristics to set the stage for the much more detailed descriptions
presented later.
Each tissue is characterized by two relaxation times: Tl and T2. Images
can be created in which either one of these two characteristics is the
predominant source of contrast. It is usually not possible to create images in
which one of the tissue characteristics (e.g., PD, T1, or T2) is the only pure
source of contrast. Typically, there is a mixing or blending of the
characteristics but an image will be more heavily weighted by one of
them. When an image is described as a T1-weighted image, this means that T1 is
the predominant source of contrast but there is also some possible contamination
from the PD and T2 characteristics.
It is
possible to produce images that show both perfusion and diffusion within tissue.
These require specific imaging methods and are often characterized as functional
imaging.
The
frequency of the RF signals emitted by tissue is affected to a small degree by
the size and characteristics of the molecules containing the magnetic nuclei.
These differences in frequencies, the chemical shift, can be displayed in
images. It is also the basis of MR spectroscopy. Spectroscopy is the process of
using magnetic resonance to analyze the chemical composition of tissue.
Spectroscopy makes use of the fact that different molecular structures have
different resonant frequencies. Typically, the MR signals from a tissue specimen
are sorted and displayed on a frequency scale. The signals from different
chemical compounds will appear as peaks along the frequency scale. This leads to
their identity and measure of relative abundance.
between the image and the three tissue characteristics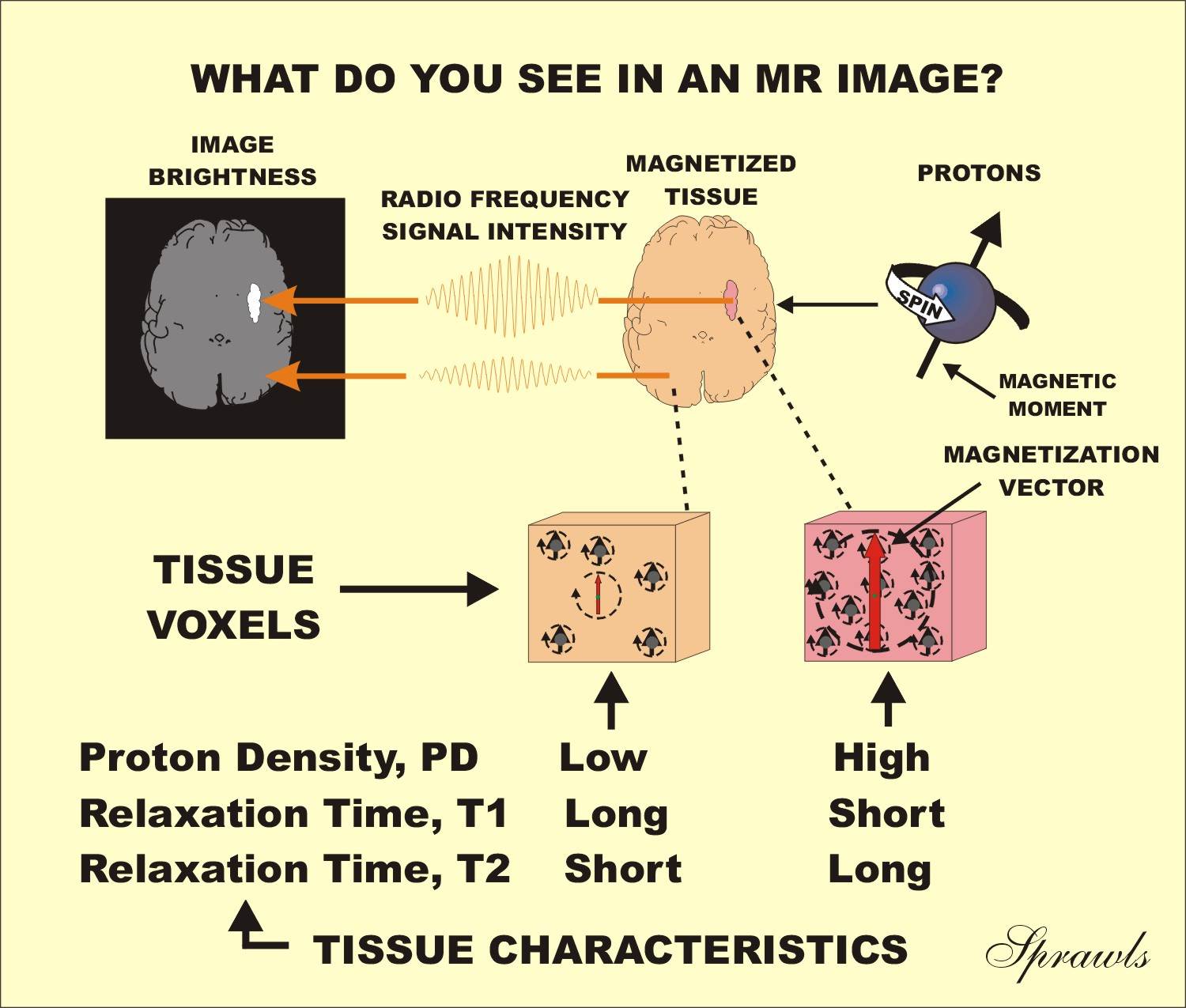
The
first thing we see in an image is RF signal intensity emitted by the tissues.
Bright areas in the image correspond to tissues that emit high signal intensity.
There are also areas in an image that appear as dark voids because no signals
are produced. Between these two extremes there will be a range of signal
intensities and shades of gray that show contrast or differences among the
various tissues.
Let us now move deeper into the imaging process and discover the
relationship between RF signal intensity and other characteristics.
The
condition within the tissue that produces the RF signal is magnetization.
At this point we will use an analogy to radioactive nuclide imaging. In nuclear
medicine procedures it is the presence of radioactivity in the tissues that
produces the radiation. In MRI it is the magnetization within the tissues that
produces the RF signal radiation displayed in the image. Therefore, when we look
at an MR image, we are seeing a display of magnetized tissue.
We will soon discover that tissue becomes magnetized when the patient is
placed in a strong magnetic field. However, all tissues are not magnetized to
the same level. During the imaging process the tissue magnetization is cycled
through a series of changes, but all tissues do not change at the same rate. It
is this difference in rates of change of the magnetization that makes the
tissues different and produces much of the useful contrast. This will be
described in much more detail later when we will learn that these rates of
change are described as magnetic relaxation times, T1 and T2.
It is the level of magnetization at specific “picture snapping” times
during the imaging procedure that determines the intensity of the resulting RF
signal and image brightness. The MR image is indeed an image of magnetized
tissue. Tissues or other materials that are not adequately magnetized during the
imaging procedure will not be visible in the image.
The
next thing we see is an image of protons that are the nuclei of hydrogen atoms.
That is why an MRI procedure is often referred to as proton imaging.
The magnetization of tissue, which produces the RF signals, comes from
protons that are actually small magnets (magnetic nuclei) present in the tissue.
These small magnets are actually the nuclei of certain atoms that have a special
magnetic property called a magnetic moment. Not all chemical substances
have an adequate abundance of magnetic nuclei.
The
only substance found in tissue that has an adequate concentration of magnetic
nuclei to produce good images is hydrogen. The nucleus of a hydrogen atom is a
single proton. Therefore, the MR image is an image of hydrogen. When tissue that
contains hydrogen (small magnetic nuclei), i.e., protons, is placed in a strong
magnetic field, some of the protons line up in the same direction as the
magnetic field. This alignment produces the magnetization in the tissue, which
then produces the RF signal. If a tissue does not have an adequate concentration
of molecules containing hydrogen, it will not be visible in an MR image.
As we
have moved deeper into the imaging process we arrive again at the three tissue
characteristics: PD, T1, and T2. It is these characteristics that we want to see
because they give us valuable information about the tissues. These
characteristics become visible because each one has an effect on the level of
magnetization that is present at the picture snapping time in each imaging
cycle. At this time we will briefly describe the effect of each and then develop
the process in more detail in Chapters 4 and 5.
When
the imaging protocol is set to produce a T1-weighted image, it is the tissues
with the short T1 values that produce the highest magnetization and are the
brightness in the image.
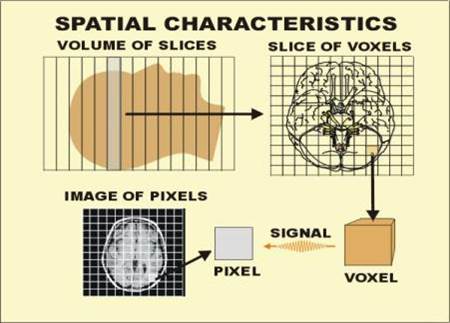
| Figure 1-3. The
spatial characteristics of MR images. |
 |
| Figure 1-4. Image
quality characteristics that can be controlled by the selection of protocol factors. |
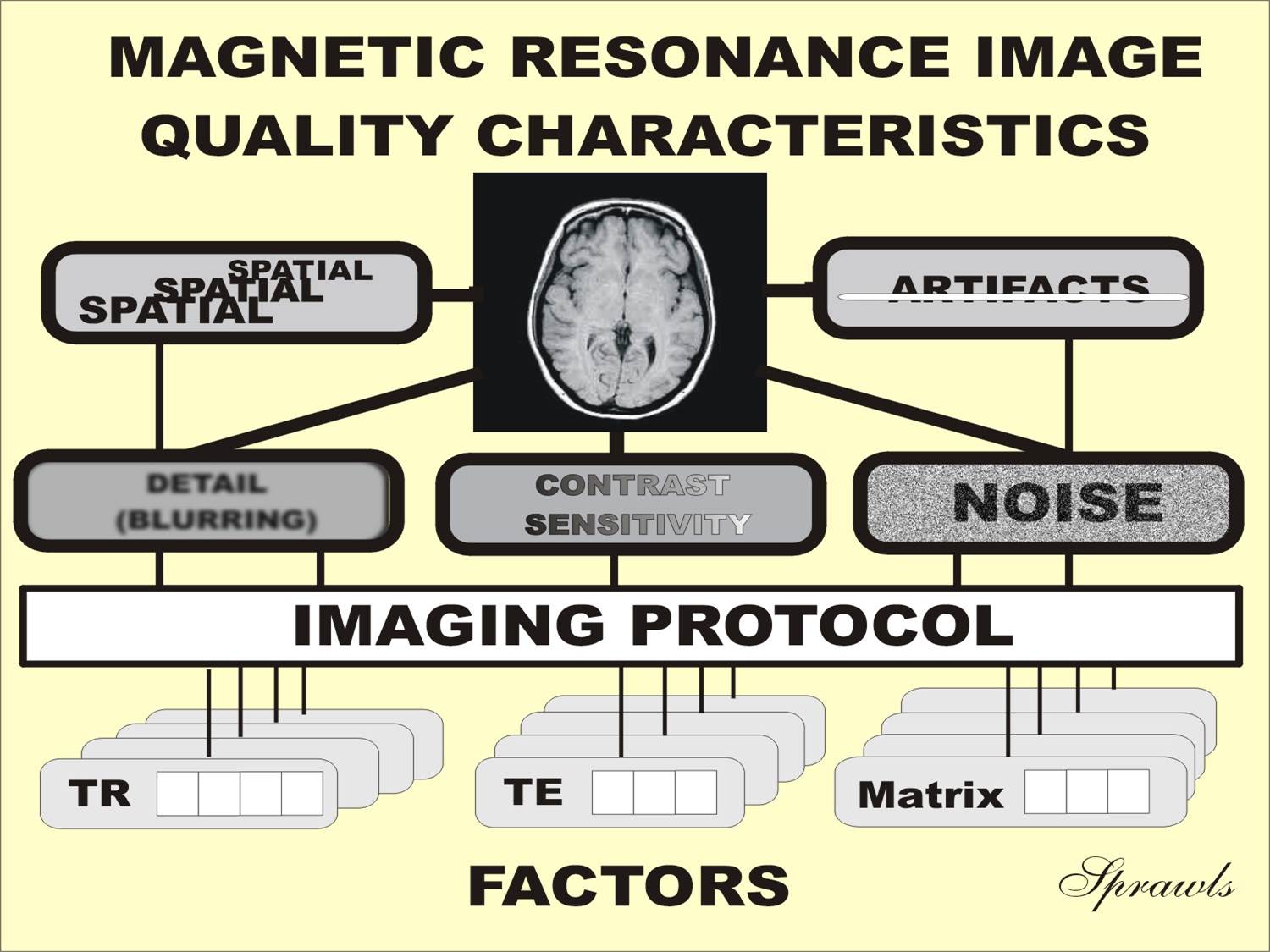 |
Not all types of clinical procedures require images with the same
characteristics. Therefore, the primary objective is to use an imaging protocol
in which the acquisition process is optimized for a specific clinical
requirement.
Although each of the image characteristics will be considered in detail
in later chapters, we will introduce them here.
Even though MRI has high contrast sensitivity relative to most of the other imaging modalities, it must be optimized for each clinical procedure. This includes the selection of the characteristics, or sources of contrast, that are to be imaged and then adjusting the protocol factors so that the sensitivity to that specific characteristic is optimized. This is illustrated in Figure 1-5.
| Figure 1-5. The
images produced when the contrast sensitivity is optimized for each of the three specific tissue characteristics. |
 |
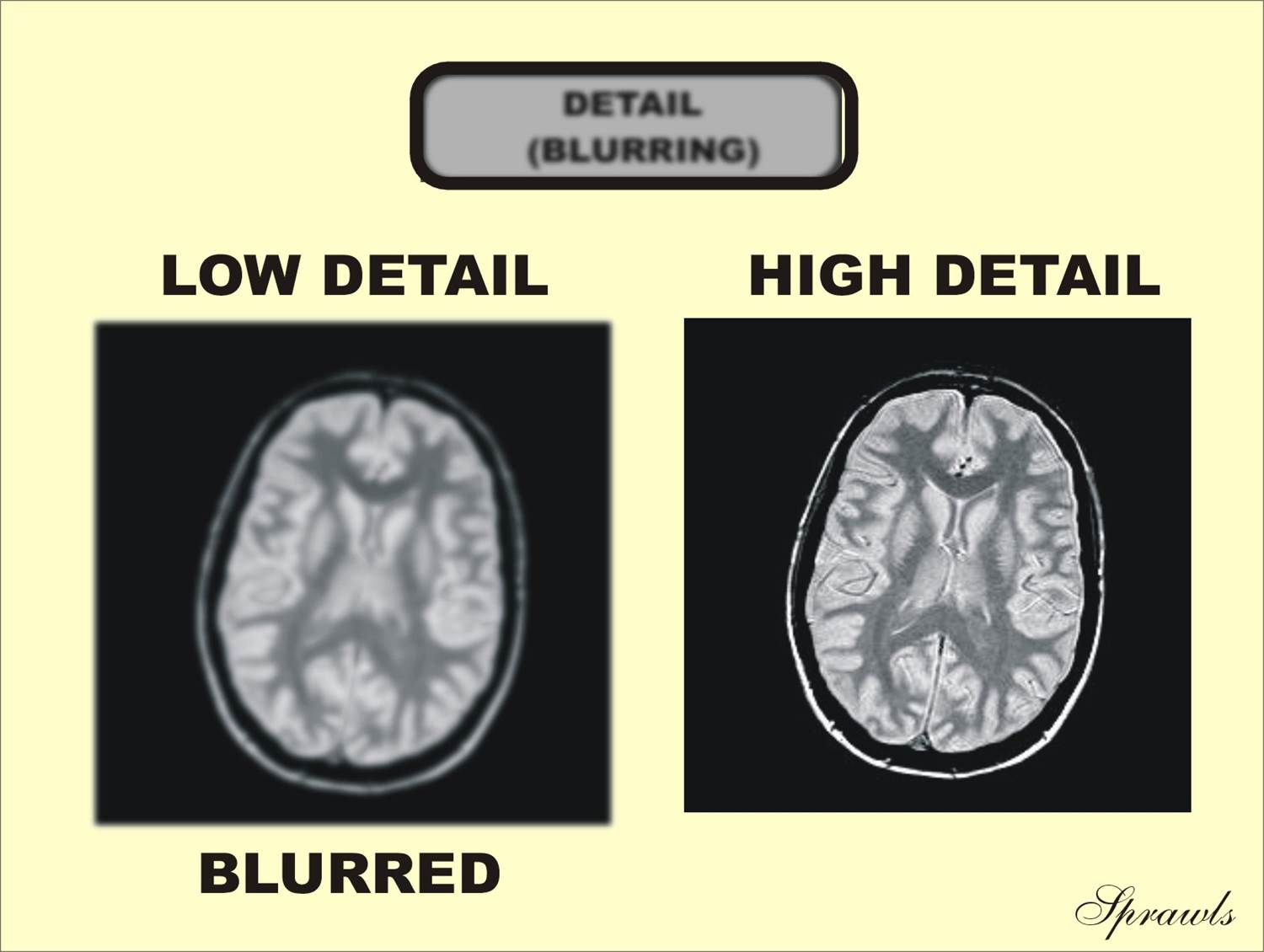
In MRI, like all modalities, the amount of blurring and the resulting
visibility of detail can be adjusted during the imaging process. Figure 1-6
shows images with different levels of blurring and visibility of detail. The
protocol factors that are used to adjust detail and the associated issues in
their optimization will be discussed in Chapter 10
| Figure 1-6. Images
with different levels of blurring and visibility of anatomical detail. |
 |
| Figure 1-7. Images
with different levels of visual noise. |
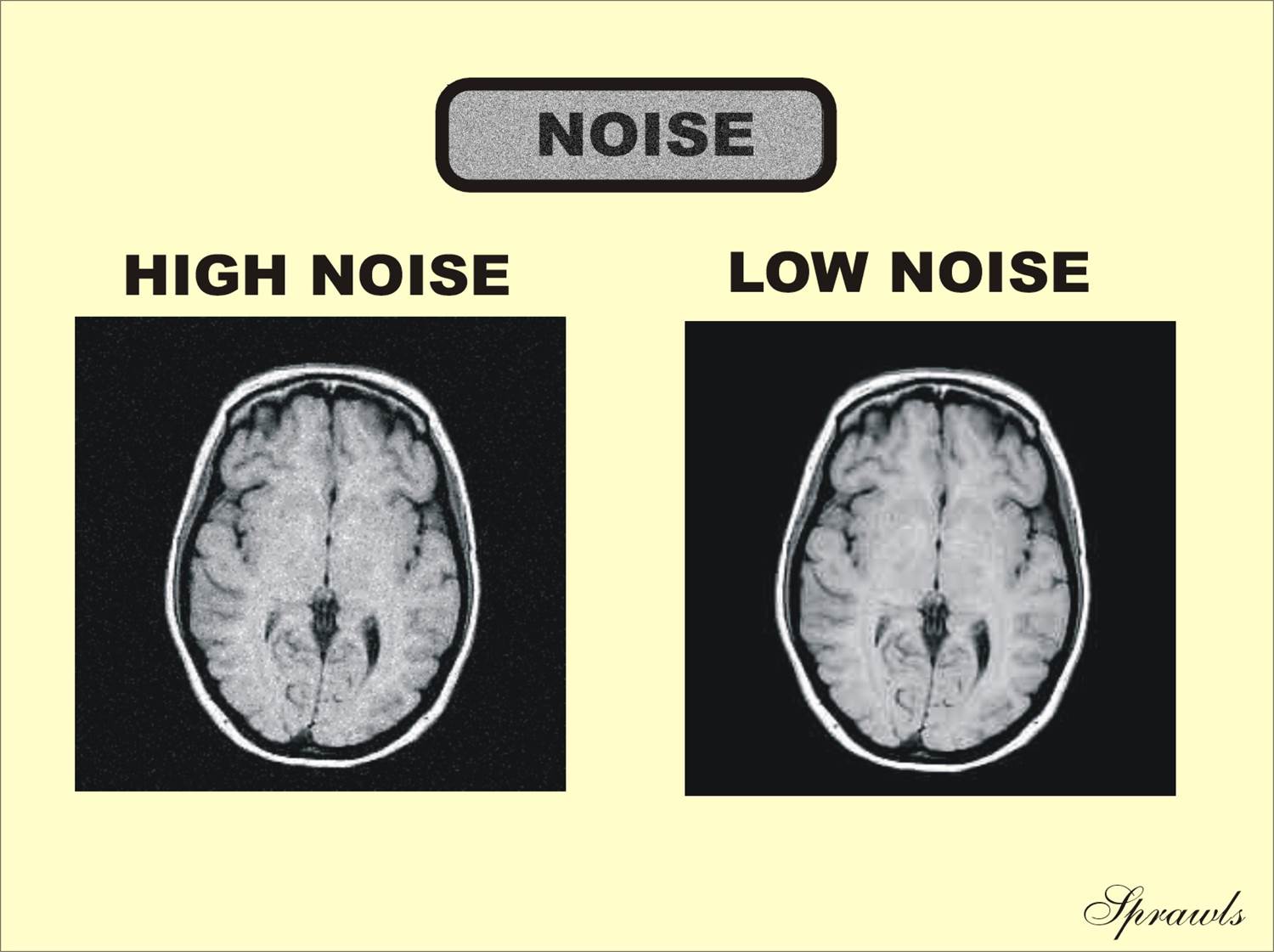 |
The amount of noise can generally be controlled through a combination of
factors as described in Chapter 10. However, many of these factors involve
compromises with other characteristics.
There is a selection of techniques that can be used to reduce the
presence of artifacts. These will be described in Chapter 14.
The
imaging protocol that is used for a specific clinical examination has a major
impact on the quality of the image and the visibility of anatomical structures
and pathologic conditions.
Therefore, the users of MRI must have a good knowledge of the imaging process
and the protocol factors and know how to set them to optimize the image
characteristics.
The
overall process of optimizing protocols will be described in Chapter 11.
Magnetic Resonance Image Characteristics
An advantage of MRI is the ability to selectively image a variety of
tissue and fluid characteristics. If a specific pathologic condition is not
visible when viewing one characteristic, there is the possibility of seeing it
by imaging some of the other characteristics.
During the imaging procedure a section of the patient’s body is divided
first into slices, and the slices are divided into a matrix of voxels. Each
voxel is an independent RF signal source. Voxel size can be adjusted and is what
determines image detail and also affects image noise.
The five major image quality characteristics—contrast sensitivity,
detail, noise, artifacts, and spatial—can be controlled to a great extent by the
settings of the various protocol factors.
MRI is a powerful diagnostic tool because the process can be optimized to
display a wide range of clinical conditions. However, maximum benefit requires a
staff with the knowledge to control the process and interpret the variety of
images.